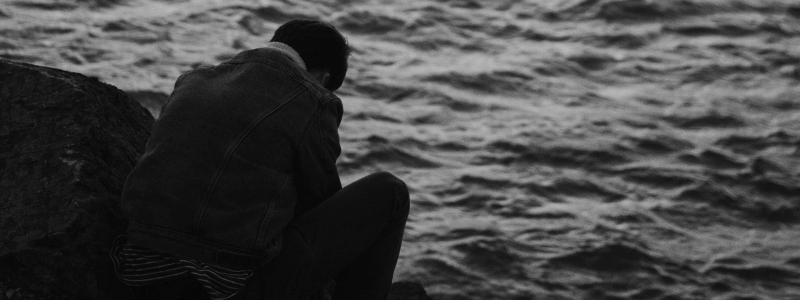
The experience of loss and grief from bereavement are often explored in psychotherapy. Finding a way to cope and move forward, when the weight of emotion feels intense. The knowledge that life ends and how we go through the associated grief is something that is hard to prepare for. Much is written about loss and grief, but from experience some common themes do emerge.
Loss is not a straight line
How do we deal with, process and manage bereavement, loss and grief? There is evidence of stages, an indication of what one might experience and how one might cope. This is always reassuring to think that we can put structure around what can feel chaotic, especially when the emotions can feel unbearable. Being able to feel that we have some control of our emotions when we are potentially overwhelmed by them. How we think about such guidance is where the challenge lies. Loss is not a straight line. The emotions surrounding it can be complex and rarely follow any neat progression. Can we be reflective, aware of how we feel and avoid pressuring ourselves to ‘move on’? Is it possible to let the emotions happen and not feel that we have to be good at how we handle death and grief?
Loss is individual
Speaking of stages and process around loss can give structure to what is going on, but can also cause us to compare ourselves to others. Seeing that everyone moves at a different pace, for whatever reason, can be hard to manage. How do we feel when others seem to be moving on, but we feel stuck? This is the point at which the individuality of death can feel most important. Everyone experiences it in a different way and thus will grieve differently. Being aware of this and resisting comparisons with others can make us feel more able to cope and less isolated with our individual experience.
Also individual is the actual response to death. The relationships that we have to the deceased always come with a different set of emotions. One person’s extreme grief can contrast with someone else’s mild sadness. Being able to express and value whatever emotional response one has is important, and ideally every response can be heard.
Loss can feel ‘ugly’
Sadness is probably the obvious emotion that comes to mind when we think of loss. Therefore, to experience anger, frustration, annoyance, and other emotions that feel a long way from sadness, isn’t easy. I once heard it described as the ‘ugly’ side of grief. It is however quite likely that one could feel any or all of these. They are hard to make sense of and hard to share with those who are also grieving. Can we share these feelings, or do they feel too challenging to be brought up? The ‘ugly’ emotions are part of grieving, so how do we find a way to acknowledge them and not feel that we are being hurtful towards the deceased or those who are also grieving?
Loss has associations
When we talk about loss and grief, it often isn’t always about one event. To grieve is to be open to a series of emotions that might take us far from what has actually happened. Past events, personal experiences, present issues can’t be neatly separated when we experience loss. Being open to this and able to acknowledge that life events don’t happen in isolation can help to frame one’s emotional response.
Loss, grief and psychotherapy
In all these reflections the common theme is that we need the space to reflect and process loss and grief. A strong support network of family and friends can be helpful. Sometimes however such a network is hard to find or speak with and at this point talking therapy can provide that reflective space. Psychotherapy for bereavement gives the bereaved the opportunity to be reflective and open with every emotion and ultimately work through their grief.
David Work is a BACP registered psychotherapist working with adults, offering long term individual psychotherapy. He works with individuals in Hove . To enquire about psychotherapy sessions with David , please contact him here, or to view our full clinical team, please click here.
Further reading by David Work –
Compulsive use of pornography